Culture & Lifestyle
Nepali society yet to embrace hard mental illnesses
Individuals with hard mental conditions are still pitied, and socially isolated.
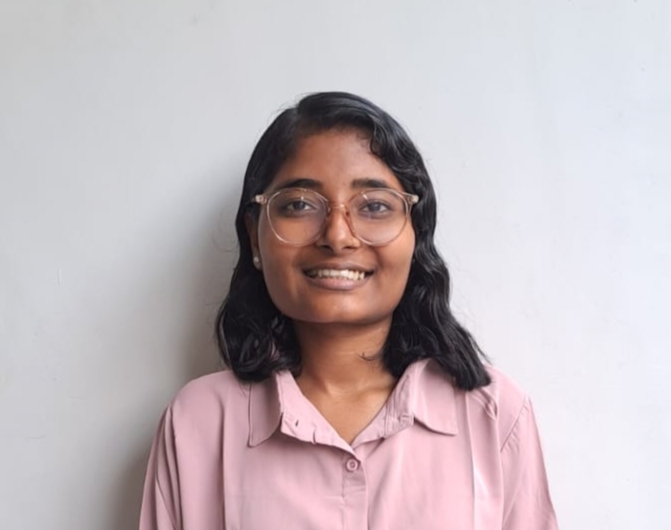
Aarati Ray
In recent years, the narrative and discourse on mental illness in Nepal have evolved significantly, making it easier for the younger generation to discuss issues like depression.
However, more severe mental disorders remain shrouded in fear and prejudice. While teenagers and young people can more readily find spaces to talk about mental health, their parents often struggle to engage in these discussions.
Dr Rishav Koirala, a psychiatrist, researcher, and executive director of the Brain and Neuroscience Center, explains that the WHO categorises mental disorders into two types. A soft mental disorder occurs when a person's insight remains intact, allowing them to distinguish between what is real and unreal. In contrast, a complex or hard mental disorder occurs when there is a risk of losing insight into reality.
People dealing with hard mental disorders are still not welcomed by society, according to Koirala. Bishnu Mahato and Padma Rai (name changed) are such individuals who have been struggling with hard mental disorders all their lives.
Mahato, a 52-year-old resident of Siraha district, has been suffering from mania and bipolar disorder. Recalling his experience, he says, “I have suffered from this mental illness since I was 16 or 17. Times were different back then. I was regarded as an anomaly.”
Mahato’s family situation was difficult; he lost his mother to suicide when he was two. Raised by his stepmother, with his father often absent, his illness went unnoticed until it became severe. “I couldn't understand what was happening to me. Everyone around me thought I was possessed by some ghostly energy,” Mahato recalls.
Koirala points out that when a condition lacks medicine or treatment, it becomes a significant concern and a source of fear. This was evident with diseases like HIV and leprosy in the past, and the same holds true for mental illness.
Seventy years ago, when there were no treatments or answers for mental illnesses, people had to be locked up and caged. Koirala also mentioned that in Dhulikhel, where Kathmandu University is now located, there used to be a prison for mentally ill patients. Those individuals were physically restrained and confined due to the lack of treatment options.
Mahato also faced similar challenges. Recalling his experience of being locked up, beaten, and spit at, he shares, “At that time, there was no knowledge of treatment in my village, so even my family had to lock me up. Looking back, there were many instances when my episodes worsened because of the mistreatment by people.”
His family was also looked down upon by society. Later, he started going to Patna, India, for treatment, as it was the only accessible mental health service. The treatment and medication in Patna did stabilise him, but due to the high dosage and side effects, he felt hollow and empty.
In 2003, when he visited Pokhara, the treatment at Manipal Hospital suited him better. Despite needing medication for the rest of his life, he is in a better and improved state, all thanks to medical and family support.
Mahato’s 16-year-old daughter adds, “Sometimes, I wish the mental health facilities available now had been present when my baba was at his lowest point. He has suffered a lot.”
According to Koirala, despite COVID normalising the space for mental health discussions, there hasn’t been much change regarding psychotic disorders (hard mental disorders).
Aevon Shrestha, a counsellor at the Center for Mental Health and Counselling-Nepal (CMC-Nepal), adds that due to the higher prejudice and discrimination against people with psychosis in rural areas, even individuals working in the mental health sector who suffer from mental illness have to hide it. There have been cases where they come to him for treatment in secret.
True to what Shrestha shared, Padma Rai (name changed), a 40-year-old from Chitwan, has to deal with her illness in secret. A counsellor and mental health practitioner, Rai has been suffering from bipolar disorder for more than 20 years.
Due to her illness, some of her colleagues mistreat her, doubting her capabilities. Rai remarked, “If even a mental health practitioner's perception can be so biased, what can we hope from others?”
Rai has faced significant challenges. In her worst episodes of bipolar disorder, she has come close to death three times and has often felt completely hopeless. “When you're dealing with an illness, it's already tough. When people start treating you differently and unfairly because of that illness, it becomes even harder.”
Every day, Rai must endure snide remarks and taunts in her own office, like, “She's crazy. Can she even work?”
Rai is frustrated by how people perceive those facing psychological disorders. She points out that when someone experiences a physical accident like a leg fracture or undergoes a medical operation like heart surgery, they often post pictures on Facebook with the status of being “under treatment”.
In response, there is an outpouring of well wishes for a speedy recovery in the comments. However, when it comes to someone struggling with a mental disorder, especially in cases of complex disorders, others tend to keep their distance, feel fearful, or neglect that person.
Rai hopes that mental health disorders can also be viewed from the same lens as physical illness. She questions why individuals facing mental illness have to be a subject of tremendous pity, strangeness, and social isolation.
There was a time when people and friends around Mahato's age would approach him to tease and make fun of him upon learning about his illness.
Circumstances have improved for Mahato, but people in his village still gossip about him being “mad.” They question and criticise his capability, hard work, and intellect. “I am tired of the word pagal (mad),” he adds.
Psychologist Alsodha Rai highlights that due to misrepresentation in movies and other media, psychotic patients are often perceived as violent and unstable individuals. However, in reality, violence is rare and can be managed effectively.
She emphasises that the support of family and loved ones is crucial for people with mental illness, as well as understanding from society at large.
Sharing how breakdowns and symptoms of individuals with severe mental illness are often exacerbated by the wrong responses from people around them or a lack of knowledge to handle the situation, she emphasizes the vital need for psycho-social counselling in today's society.
According to her, psycho-social counselling can reduce stigma and help family members and friends of individuals struggling with mental illness become an effective support system.
But change still seems to be far away.
Mahato's daughter mentions that even now, discussing mental illness is more comfortable with her age group compared to her father's generation. She adds, "I have seen how anxious he gets when someone sees his medicine or when he has to buy medicine from some new shop. I hope that society changes to an extent where my baba and people of his age group can openly discuss and understand mental health in a supportive environment."




 10.12°C Kathmandu
10.12°C Kathmandu