Life & Style
How PCOS affects the skin
Dermatologist Prativa Shrestha talks about the skin conditions linked to polycystic ovary syndrome..jpg&w=900&height=601)
Aarati Ray
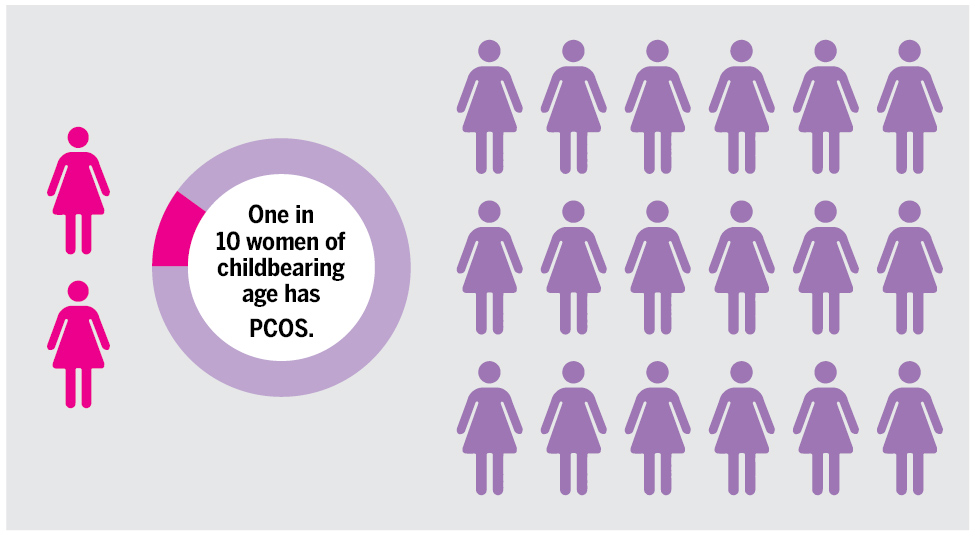
Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects people with ovaries and often leads to an imbalance in sex hormones, particularly an increased level of androgens (male hormones). This hormonal imbalance can show up on the skin in different ways, like causing acne, excess hair growth or oily skin. According to the Office on Women’s Health, one in every ten women of childbearing age has PCOS.
Dermatologist Dr Prativa Shrestha, shares how PCOS and skin diseases are connected.

What are some common skin problems seen in people with PCOS?
The common skin problems associated with PCOS are either due to hyperandrogenism, ie excess male hormone or hyperinsulinemia, ie an increase in blood insulin level.
Symptoms due to hyperandrogenism are oily skin and scalp, pimples—especially in the lower half of the face, increased unwanted thick dark facial and body hair, and scalp hair thinning, whereas darkening and thickening of the skin fold such as the neck, underarms, and groin are due to hyperinsulinemia.
How does the hormone imbalance due to PCOS cause skin problems?
PCOS is a complicated problem because hormones are not balanced. Women usually have some male hormones, but in PCOS, these hormones become too high, affecting the body’s normal functions.
Male hormones influence the transition of soft, light and less pigmented hair into dark, thick, pigmented hair in areas such as the upper lip, chin, middle of the chest, back, upper and lower abdomen, and upper arm. It makes the glands that produce oil work too much, leading to the skin and scalp becoming oily. This can cause pimples, mainly on the lower face, chest and upper back.
In the scalp, it makes hair thin, short and less coloured, a process called miniaturisation. Insulin is the hormone that processes glucose in the cell. In insulin resistance, insulin is unable to process the glucose, and excess glucose imposes a risk for diabetes, high cholesterol and cardiovascular disease.
Insulin also causes the skin in the folds—such as the neck, underarm, groin, etc—to become pigmented and velvety, known as acanthosis nigricans. The presence of acanthosis nigricans can be a clinical marker for underlying hyperinsulinemia and its potential risk.
What challenges do patients with PCOS-related skin issues commonly face?
Pimples are a common problem, but in PCOS, they are difficult to treat. They are likely to develop severe papulopustular lesions. Due to an ongoing underlying hormonal imbalance, they are difficult to clear, have the potential to leave acne scars, and are likely to reoccur.
There isn’t an effective topical or oral medical treatment for hirsutism. It needs laser hair removal. The need to do it at regular intervals and the cost might be an issue for many clients.
Are there specific skincare routines or lifestyle changes that can benefit these patients?
There is no specific skincare routine for such patients, as each case is unique and requires a different approach. In general, choosing a product that is fragrance-free, non-comedogenic and silicon-free is helpful as it is less likely to clog pores and cause acne. Those PCOS clients taking oral contraceptive pills should follow strict sun protection and wear broad-spectrum sunscreen daily as recommended to avoid melasma.
Lifestyle changes play a huge role in the management of PCOS. Hormonal imbalance causes easy weight gain, specifically central fat. And the extra fat deposition causes further hormonal imbalance, so it is a self-perpetuating vicious cycle. I would highly recommend good sleep, stress reduction, mindful eating with a high-fibre and protein diet, and regular exercise help to keep PCOS under control.
How do you collaborate with gynaecologists or endocrinologists to manage PCOS-related skin issues?
The management of PCOS requires a multidisciplinary approach. When I suspect a client of having PCOS, I encourage them to visit a gynaecologist and an endocrinologist. An approach to lean PCOS versus obese PCOS is different, and its management requires nutritionist consultation.
Many teen girls fail to understand PCOS and skin disorders and have low self-esteem because of the skin disorders. How can family members help in this case?
It is normal to have irregular periods and acne in the first year after starting menarche. So, girls don’t need to visit a gynaecologist or a dermatologist due to this.
You are likely to have an irregular period if you have one cycle in more than 90 days after a year of menarche, if your cycle occurs in less than 21 days or more than 45 days in the first three years of menarche, or if you are having less than eight cycles per year after three years of menarche. So, if you consistently have irregular periods and intense acne, visit your doctor for further analysis.
PCOS is an incurable condition that affects women in various aspects of life. It affects their self-esteem, sleep, mood and eating habits. The continuous support of the family is always necessary for someone with PCOS’ emotional and physical well-being.




 9.88°C Kathmandu
9.88°C Kathmandu