Opinion
Risks of zoonoses
There should be greater awareness about the origin and transmission of these diseases to prevent an epidemic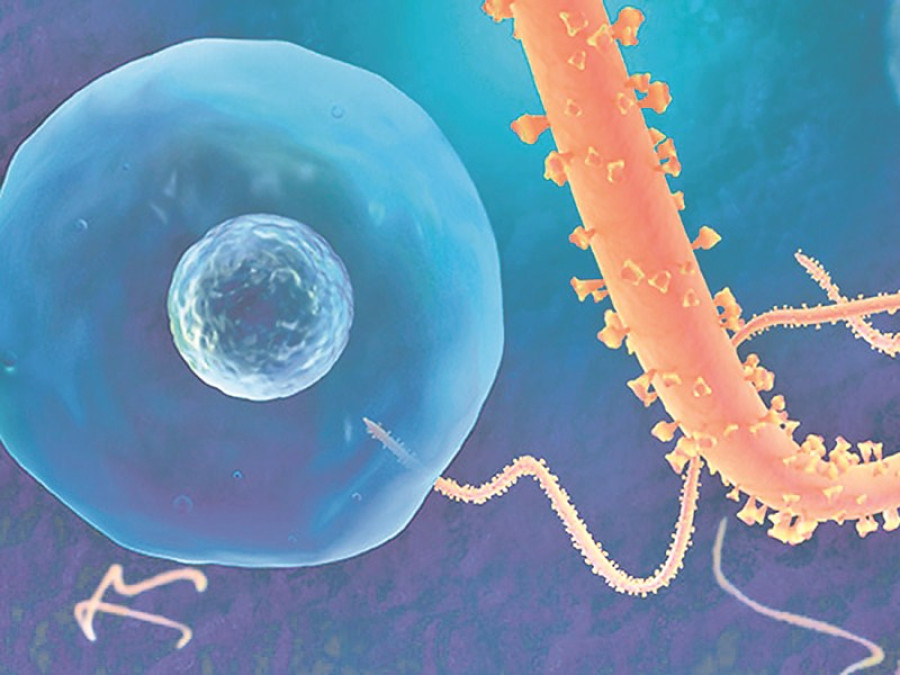
Nirajan Niroula
Zoonoses are diseases that can transmit between humans and animals. While this is the most common notion regarding the zoonotic diseases, they fit a wide array of situations. Diseases like Ebola and hantavirus have animals as their primary hosts. For other diseases like salmonellosis and tuberculosis, both humans and animals are primary hosts. For some other diseases, whose primary hosts are animals, transmission to humans occurs only to meet a dead end and there is no further proliferation. Diseases like anthrax, west-nile fever, rabies, etc. fall in this category. Many lethal diseases that afflict humans today were historically found exclusively in animals. Somehow, they transcended the cross-species barrier to affect human beings as well. Prominent examples include HIV/AIDS, Influenza A and Sars (Severe Acute Respiratory Syndrome).
Most of the zoonoses have either a bacterial or viral aetiology (cause or origin). However, zoonotic diseases are also associated with certain prions, protozoa, fungi and even helminths (parasitic worms). Disease begins when the causative agent of a zoonosis enters a human host. The route of transmission could be direct contact with sick or reservoir animals, contaminated food or water, and so on.
According to research, more than 60 percent of pathogenic organisms are zoonotic in nature. The World Health Organisation (WHO) asserts that pathogens responsible for more than threefourth of new diseases affecting humans over the past decade have an animal origin. In the wake of Ebola and pandemic Influenza A outbreaks, the scientific community has foreboded that any ‘World War Z’-like scenario would be brought about by these types of viral
zoonoses. In order to facilitate early detection and warning of imminent pandemics, the WHO, the World Organisation for Animal Health (OIE) and the Food and Agriculture Organisation (FAO) have jointly formed a Global Early Warning System (GLEWS) for major animal diseases, including zoonoses. The goal of GLEWS is to inform prevention and control measures through the rapid detection and risk assessment of health threats and events of potential concern at the human-animal-ecosystems interface.
Risks and emergence
People close to animals are more susceptible to zoonotic diseases. Given the close association of livestock and humans in rural Nepal, the odds of farmers being infected by zoonotic diseases are high. Likewise, veterinarians and para-veterinarians are highly susceptible due to their exposure to sick animals. Children are at high risks of contracting canine or feline worms from their pets. Since some wild animals and birds are reservoir hosts for many lethal pathogens, people living around the wildlife-human interface region such as buffer zones of protected areas are also at a greater risk. The outbreak of Ebola in West African countries provides evidence of this. Likewise, detection of Mycobacterium tuberculosis bacteria in elephants and their mahouts around the Chitwan National park is an intriguing issue for global zoonoses researchers.
The WHO defines emerging zoonoses as ‘a zoonosis that is newly recognised or newly evolved, or has occurred previously, but shows increases in incidence or expansion in a geographic, host or vector range. Some of these diseases may further evolve and become effectively and essentially transmissible from human to human.’ Two basic ideas explain the re-emergence of diseases, the first being the increased virulence of the etiological agent and the second being the increased susceptibility of the host augmented by environmental changes. Ebola, hantavirus, Nipah virus, avian influenza, swine influenza, etc are emerging zoonotic diseases. Tuberculosis, brucellosis, rabies, cysticercosis, etc are re-emerging zoonotic diseases. Scientists believe that disease emergence and re-emergence are due to the evolutionary response to changes in the environment, including anthropogenic factors such as new agricultural practices, urbanisation, globalisation, as well as climate change.
Unsafe practices
Due to the lack of studies on the incidence and prevalence of zoonotic diseases, a clear picture about them cannot be drawn. However, a few studies that have been conducted show that many common zoonotic diseases are present at an alarming proportion. Some of our cultural and traditional practices are making us more susceptible to the zoonotic diseases. Examples include the practice of drinking raw yak blood on some propitious occasions in the Himalayas, the drinking of cow urine during some Hindu religious ceremonies and consumption of Panchamrit made out of raw milk and dairy products. In some parts of the Far West, yogurt and buttermilk are still made from raw milk. Consumption of such
products increases the chances of being infected by milk-borne diseases. This is because raw milk from infected animals almost always contains infection-causing bacteria or virus.
In some communities, cuisines made out of raw meat is considered a delicacy. However, some people are probably aware of the threats posed by such food. There are serious repercussions of eating raw, partially cooked or contaminated meat. Creutzfeldt-Jakob disease and Hemolytic Uremic Syndrome, a serious bacterial disease common in the United States, are some of them.
In Nepal, many people are still unbeknownst of the possible transmission of diseases from animals. We are, it appears, ill-prepared to curb an epidemic on our own. So it is high time we made people aware of the possible routes of transmission, improve our vigilance and reporting mechanisms, and consolidate our resources to reduce the chances of a zoonotic epidemic.
Niroula is a veterinary medicine graduate from the Institute of Agriculture and Animal Science, Chitwan




 12.12°C Kathmandu
12.12°C Kathmandu