Opinion
Time for change
To provide quality healthcare to patients, doctors should be able to focus on clinical care
Bikash Gauchan & Ryan Schwarz
An 18-year-old girl from a remote part of Mugu district walks for two days to reach the Gamgadhi District Hospital with four days of heavy vaginal bleeding and no menstrual period for three months. At the hospital, the one doctor present recommends Manual Vacuum Aspiration (MVA)—the standard procedure for the management of incomplete abortion. But as the doctor prepares for the procedure, he realises the hospital lacks the necessary equipment. Additionally, the doctor wants to give her blood, but the hospital also lacks blood transfusion capacity. He then refers her to a higher centre, but she has no money for transportation, and tragically, five days later she dies from heavy blood loss.
This story is fictional, but not far from reality. Similar cases are encountered in district hospitals throughout rural Nepal every day. What can we do to prevent them? Let us first begin with the problem which creates this situation.
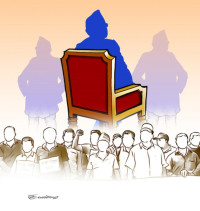
District and zonal hospitals in Nepal are run under the leadership of the Medical Superintendent (MS)—usually a doctor. While the MSs are well-trained in clinical medicine and can provide high quality care to their patients, they are not trained in administration, finance, procurement, facilities management, human resources, or policy, all of which are vital components to run a hospital. The complexities and challenges of the MS’s role are tremendous, and the healthcare system provides them limited support.
District hospitals are staffed usually with only one or two doctors and, despite the Ministry of Health’s (MoH) ongoing efforts at improvement, are significantly under-staffed to provide quality care for their patients. More importantly, in addition to their clinical roles, the MS must also oversee the administrative, financial, data monitoring, procurement, and HR functions in the hospital, as well as all public health programmes throughout the district, including health posts and primary health centres. With responsibilities as broad and challenging as this, it is not surprising that many hospitals throughout Nepal are unable to provide necessary treatments or blood transfusions.
A novel model
In Achham district, at Bayalpata Hospital—a public-private partnership between the MoH and Nyaya Health Nepal—we are experimenting with a different management model. Where the standard hospital management model expects the MS to oversee a wide range of responsibilities that they have not been properly trained in, our management model employs a team-based approach. A Medical Director, instead of the MS, works closely with non-clinicians in finance, logistics, procurement, human resource management and policy, to share management responsibilities as a directorial team. This approach enables our team to develop logistics and finance systems, as well as employee and partnership policy, ultimately resulting in higher benefits for the patients we serve. In parallel, it has enabled our Medical Director, and other clinicians working under him, to focus their time and efforts on continual improvement of the clinical services we offer—providing the patients the best care possible.
Recently, a 20-year-old girl arrived at Bayalpata Hospital. Similar to the hypothetical case above, she was bleeding severely and at great risk of death. It was the system set up by our Logistics and Procurement teams that made sure there was necessary equipment for blood transfusion and back-up solar power for the Operation Theater at night-time, enabling the medical staff to focus their efforts wholly on the patient.
Constitutional right
With the promulgation of Nepal’s constitution, the public has been guaranteed the right of basic healthcare, free of cost. It is a wonderful moment in the country’s history, yet also a challenging one for a healthcare system that already struggles to deliver quality care. To ensure the country can provide good healthcare, doctors should be able to focus on clinical care, and get the support they need. The MS model unfairly requires of doctors responsibilities that they do not have the necessary training or resources for. Just as we do not expect finance managers to perform surgery, doctors should not be performing managerial tasks and should be able to focus their efforts on providing the life-saving care they are trained for. Nepali history is at a crossroads, and as we build the Nepal of tomorrow, we must reconsider what management models offer the best to the public sector systems that serve its people.
Gauchan is the Medical Director for Bayalpata Hospital in Achham; Schwarz is the Chief Operating Officer for Possible, an NGO, and is resident physician in Internal Medicine & Pediatrics at Harvard Medical School




 18.12°C Kathmandu
18.12°C Kathmandu