Columns
The culprit behind black fungus
Stricter adherence to infection control policies can help contain infectious diseases.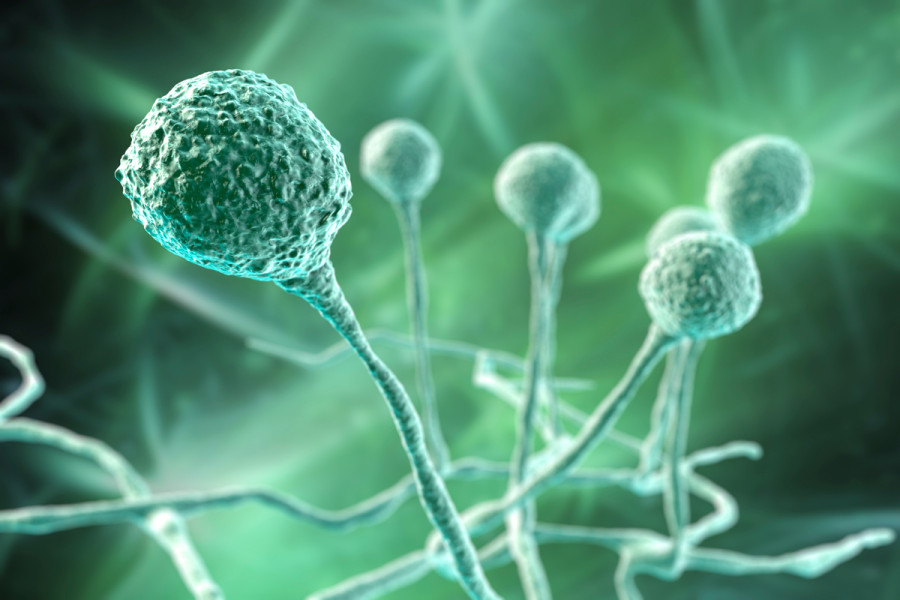
Balmukunda Regmi
During the second wave of the Cororonavirus epidemic in South Asia, another deadly infection caused by opportunistic fungus mucormycete, commonly known as black fungus, emerged as a public health threat in Nepal, India and many parts of the world. Despite extensive vaccinations against Covid-19, the recent increase in coronavirus cases points to the possibility that we may face a third wave, mainly propelled by the Omicron variant. So far, Omicron seems less deadly than the delta variant and responsive primarily to the available vaccines and clinical management. However, as with the second wave, the possibility of the spread of mucormycosis associated with the third wave cannot be ruled out.
Reasons for the coronavirus infection-related weak immunity, opportunistic infections and recommended precautions remain unchanged. But, as I had postulated in a previous article published in The Kathmandu Post, subsequent Indian studies did not establish a correlation between the widely blamed industrial use of oxygen cylinders and the spread of the black fungus.
Air conditioning (AC) units as the reservoirs of fungal spores have been long-known. Early in 2002, a study by Hamada and Fujita published in the journal Atmospheric Environment showed the average fungal contamination of AC filters was about 5-fold greater than that of a carpet, and Cladosporium and Penicillium were predominant in AC filters. A 2005 study conducted by Kelkar, Bal and Kulkarni was published in the Journal of Hospital Infection. Based on the evaluations of Operating Theatre AC units in 25 Indian hospitals, the overall rate of fungal colonisation of the AC filters was 26 percent. It concluded postoperative fungal infections might be caused by the discharge of spores from contaminated AC units.
Based on their studies in Neonatal High Dependency Units and Neonatal Intensive Care Units in Poland, Gniadek et al. report in the 2020 issue of Annals of Agricultural and Environmental Medicine, fungal growth was observed on 60 percent of samples collected from ward furnishings and 7 percent of samples collected from medical equipment.
According to a 2021 November article published in Scroll.in, mucormycosis was spread by contamination of air conditioning vents of hospitals in India. In quoting Dr Arunaloke Chakrabarti, head of the Post Graduate Institute of Medical Education and Research in Chandigarh Microbiology department. The report states, samples were collected from oxygen cylinders, storage tanks and air-conditioning vents of 11 tertiary care hospitals where mucormycosis patients were treated. They found fungal spores in 11 percent of samples collected from air-conditioning vents, but no spores were found in samples taken from oxygen cylinders or humidifiers. Chakrabarti says, “We could directly correlate this with high mucormycosis cases in those hospitals.”
Implications
These findings have important implications. First, the cooperation between basic sciences and clinical practices should be strengthened, and research in basic sciences and their findings should be emphasised. Logical extensions of such results and their careful clinical evaluations and tests contribute to clearing myths and developing new methods, medicines and practices.
Second, during the second wave of the Coronavirus pandemic, humanity faced mucormycosis as the dominant opportunistic fungal threat. Already published studies indicate the possibility of outbreaks of other fungal and other microbial infections any time in future.
Third, our establishments, including the medical field, are not sufficiently critical in thinking. Against all odds, oxygen and water were supposed to be responsible for forming mucormycete spores. No attention was given to the fact that there is no evidence of the fungus growing in water or hyperbaric oxygen. This again calls for a multidisciplinary approach.
Fourth, our cleanly-looking hospitals, medical devices, instruments and health workers are less so in terms of deadly microorganisms. A 2020 Rwandan study showed, all sampled electronic devices used by healthcare workers (HCWs) at Ruhengeri Referral Hospital within four different units: maternity, neonatology, intensive care, and theatre room were contaminated with either single or mixed bacterial agents. Albrich and Harbarth write in Lancet (2008) that the transmission may occur from colonised HCWs and actively infected ones. Multidrug-resistant bacteria MRSA, extended-spectrum beta-lactamase-producing Enterobacteriaceae, carbapenemase-producing Enterobacteriaceae and vancomycin-resistant enterococci rarely cause infections in HCWs but may cause significant morbidity in patients.
Fifth, when we combine this background information with the fact that nosocomial infections are more hazardous to public health, these bugs tend to be more multidrug-resistant strains than their counterparts found in the communities. Hence unnecessary visits to clinics and hospitals admissions should be discouraged. A WHO report says a literature review of national or multicentre studies published from 1995-2008. The overall prevalence of hospital-acquired infections in developed countries varies between 5.1 percent and 11.6 percent, and approximately the same proportion of hospitalised patients acquire at least one condition. It says, developing countries have markedly higher hospital-wide infection rates.
Prudence necessary
Clients visiting clinical facilities with a purpose other than consulting the obstetricians or getting immunisation vaccines are themselves patients and thus find it difficult to distinguish between their pre-existing and hospital-acquired diseases. Due to ignorance on the part of patients and that of healthcare workers, many nosocomial infections are simply not considered nosocomial. There are provisions for separate dedicated hospitals or wards to manage infectious diseases, but it will never be enough to separate the average population from infected ones.
However, strict adherence to infection control policies on all stakeholders, including the public, policymakers, patients, carriers, HCWs, hospital and clinic management, waste management and disposal authorities and workers, can help contain infectious diseases. A culture of open disclosure of the status of all infected people and a reciprocal respectful, kind, philanthropic, humane response to their needs by the whole community is necessary to avoid preventable transmission of the infections.
At a personal level, Saloojee and Stenhoff suggest, HCWs can help minimise the cross infections and protect patients by thoroughly adhering to hand proper washing practice, properly cleaning and using gloves, masks, gowns, stethoscopes, white coats and intravenous catheters. However, such practices need adequate institutional support and a good infrastructure. In developing countries like Nepal, hospitals often face shortages of clean water, soap and paper towels, which curtail fundamental infection control activities. Policies without technical and financial backings make little difference, although they can contribute significantly.
Given limited resources, socialistic national infrastructure and physical facility policies need to be developed and enforced. Take ACs, for example. These machines are of no real value in cities like Kathmandu and Pokhara. We should consider banning these and similar stuff in most healthcare facilities, public or private. Rather than investing in creating a clean private room, both the public and private money should be invested to benefit all people, such as waste management, environmental protection and infection control. To nourish a plant, one should water the roots, not its leaves.




 21.12°C Kathmandu
21.12°C Kathmandu















